This blog covers important fertility hormones tests, when in your menstrual cycle to test them, and the difference between Clinical and Optimal results.
When taking longer than you expect to get pregnant it can be really helpful to dig a little deeper to learn more about your body, hormone levels and if key nutrients your body needs. It can however also be a bit overwhelming to know which fertility tests to speak to your GP about.
In this blog I am not going to list every fertility test there is. Instead, I am going to cover key tests which can tell you what’s happening with your hormones, and if you have sufficient levels of important nutrients required for conception and a healthy pregnancy. Then, when you talk to your GP, you will have a better idea of the tests your doctor might suggest when you are trying to get pregnant. Sometimes the NHS recommend you see your GP when trying for a baby if you have a long-term conditions such as diabetes, if there is a risk of passing on sickle cell or you regularly take medicines, as all of these can affect future pregnancies.
Dance of your Hormones
Your hormone levels fluctuate throughout your menstrual cycle, and having optimal of specific hormones at key times during your cycle is really important for getting and staying pregnant.
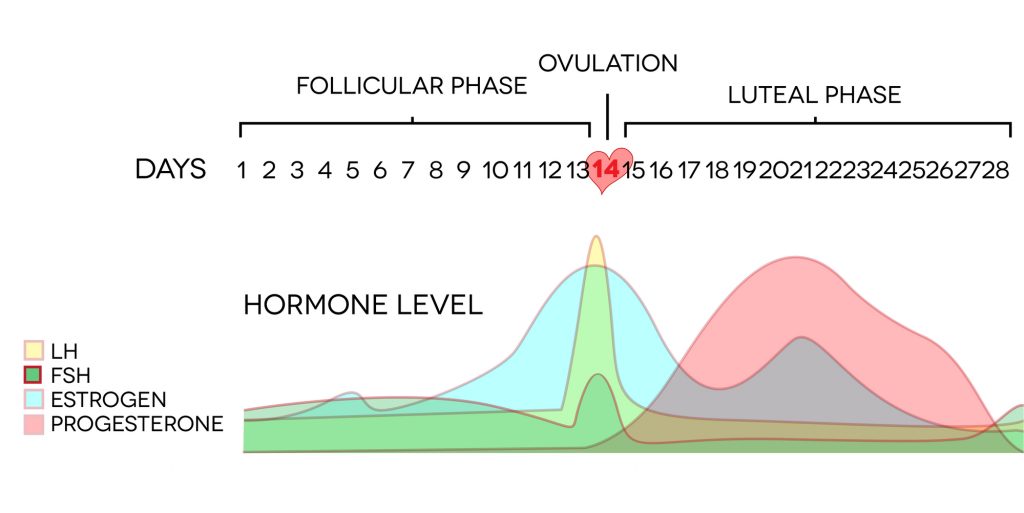
Day 3 Hormone Panel
This is a blood test taken on the 3rd (sometimes 2nd) day after your period has started. This is considered to be a baseline test to assess hormone levels and, importantly, their ratios between each other at the start of the Follicular phase of your menstrual cycle. Oestrogen, Luteinising Hormone, Follicle Stimulating Hormone are all tested along with other markers such as Testosterone, SHGB and Prolactin. AMH (Anti-Müllerian hormone) levels might also be tested at this point. Like the other hormones tested, levels can change from cycle to cycle. This test is seen by some professionals to be controversial. AMH is a marker of egg reserves but is, in fact, not the most accurate marker of fertility. AMH is however an important marker for POI (Premature Ovarian Insufficiency) and PCOS (Polycystic Ovarian Syndrome).
Day 21 Progesterone Test
This blood test is taken on Day 21 of your menstrual cycle to assess your level of Progesterone when it is expected to be the highest in your cycle: 7 days after ovulation. That is, of course, if you ovulate on Day 14, which many women don’t; and you might not either. If that is the case ,a Day 21 test will not provide an accurate result. Getting to know your body better and determining the day you ovulate will help you pinpoint the most accurate day of your cycle to test your progesterone levels.
The NHS regard a result of >30 nmol/L Serum Progesterone as an indication that you have ovulated during that particular cycle. Best practice is to test each month for 3 consecutive cycles. In clinic, I only see this additional testing happen on the NHS when the first cycle result is < 30nmol/L.
Ideally Progesterone will stay elevated for at least 10 days after ovulation; and when it drops, this will dovetail with the arrival of your period. After conception your Progesterone levels stay raised, so for those of you using an Ovulation APP or charting BBT you will see a thermal rise and this will stay elevated for your pregnancy.

Why we need Folate, Vitamin B12 & Vitamin D for Conception and Pregnancy
Folate (Vitamin B9), Vitamin B12 and Vitamin D are essential for conception, implantation and maintaining a healthy pregnancy. Your GP will test for these alongside your Day 3 hormone panel.
Folate is essential for making and repairing tissues, DNA and producing healthy red blood cells. All crucial for growing a new baby! The synthetic form of Folate is called Folic Acid. The NHS recommend women take 400 µg (micrograms) of folic acid when trying to conceive and during the first 12 weeks of pregnancy For certain health conditions, including Coeliac Disease, Crohn’s Disease, Ulcerative Colitis, and patients who have had bariatric surgery and potential problems with folate absorption, and if your BMI is >35, then 5mg folic acid is recommended.
However, Folic Acid is not readily absorbed in the body. Many pregnancy pre-natal supplements contain Methyl-folate: a form of Folate which is more bioavailable. Ensure your pregnancy supplement contains at least 400 micrograms. Folate is water soluble, so can’t be stored easily in the body. Therefore, it is important to have a regular intake from your diet. Foods that contain folate include: barley, beans and peas, eggs, endive, green leafy vegetables, lentils, liver, organ meats, sprouts, soybeans and yeast.
When testing blood levels of Folate, it is important to test serum levels (how much Folate is in the blood) AND Red Cell Folate (how much Folate is in the cells and reaching parts of the body). However, your GP only tends to request Red Cell Folate if you present with certain symptoms of deficiency and a Vitamin B12 deficiency has already been ruled out.
Vitamin B12 is needed to make new blood cells and tissues, cellular repair and for nerve health. Your GP will test Total Serum Vitamin B12: the level of Vitamin B12 in the liquid portion of your blood. However, in Functional Nutrition we always want to know the level of Active Vitamin B12: how much Vitamin B12 is readily available for your body to use.
Sources of vitamin B12 are mainly found in animal products and include red meat, fish, poultry, milk, and eggs. Therefore, Vegans and some Vegetarians must take Vitamin B12 supplements to provide the body with adequate levels of B12.
Folate and Vitamin B12 are frequently measured alongside a Full Blood Count (FBC) which your GP may also test as standard, but especially if you have symptoms of anaemia. It is important to know taking Folate on its own can mask Vitamin B12 deficiency.
Vitamin D is interesting because it is actually a fat-soluble hormone, and not a Vitamin at all! It is needed to support many biochemical reactions. Here we are focussing specifically on fertility and pregnancy; but Vitamin D is also important for bone & muscle health, cardiovascular health and brain health.. It also regulates calcium and phosphate metabolism in the body. Specifically for fertility and pregnancy, low levels of Vitamin D are linked to lower fertility rates and pregnancy complications including low birth weight, pre-eclampsia, neonatal mortality and infant asthma.
NHS guidance is to take 400 IU Vitamin D per day (the equivalent of 10 micrograms) during winter months. This is aimed to prevent deficiency; however, much higher amounts of Vitamin D are needed to maintain optimal levels, especially during the winter when there is less sun exposure, and for people with genetic traits that make it harder for them to metabolise Vitamin D.
I frequently hear from clients that their GP refuses to test their Vitamin D level. The NHS do offer a postal Vitamin D test as a finger prick test for £31.
I also hear how difficult it is to get a GP appointment; and when you do, they might not be willing to run the tests you request for fertility investigations, especially if there are no obvious clinical symptoms. If you choose to order blood tests privately, it is important to find someone who is qualified to help you order the tests, explain the results, and importantly tell you what you can do to optimise your results. They will also be trained to contact your GP to let them know if any of the results are out of range and so your GP knows about this.
The difference between Optimal and Clinical results?
In Functional Nutrition, blood test results are considered optimal when they allow the body’s biochemical pathways and processes to work effectively and maximise health and vitality. These differ from the Clinical ranges the NHS use, which tend to be much broader and will inform your doctor if medical intervention or treatment is necessary. Let’s take a look at result ranges for Folate, Vitamin B12 and Vitamin D.
Folate
Serum Folate is considered clinically low at 7–10 nmol/L (3–4.5 µg/L), where <7 nmol/L indicates folate deficiency. The optimal range for Serum Folate is higher at 27-38.5 nmol/L (12-17 µg/L) . The clinical range for Red Cell Folate is 340 – 1474.7 nmol/L with anything < 340 nmol/L (150 µg/L) consistent with clinical folate deficiency (in the absence of vitamin B12 deficiency). Optimal Red Cell Folate is considered to be 500-1500 nmol/L.
Vitamin B12
Clinically low levels of Serum Vitamin B12 are <200 nanograms/L and your GP will want to know if they are this low. Very often at this level, and depending on the health reasons causing this, you may be prescribed Vitamin B12 in the form of as Hydroxocobalamin injections. However, Functional Nutrition regards levels of Vitamin B12 to be 700-1000 nanograms/L to be at a level for your body systems to function optimally. Anything lower is considered sub-optimal and usually addressed with diet, supplements and increasing sun exposure.
Vitamin D
Vitamin D (25 OH) is considered insufficient when lower than <50 nmoles/L, and considered deficient if lower than where <25 nmoles/L . The optimal range is between 75-120 nmoles/L.
For all of these results, it is a Goldilocks scenario. You want to aim for your levels to be optimal but not overly high, as when the levels are out of balance, this can start to impact other functions in the body. For example, if Vitamin D levels are too high, this can lower your body’s natural Melatonin levels and impact on sleep, egg development and endometrial health. Also, if you are supplementing with Vitamin D and your blood levels continue to stay low, this may be a sign of insufficient cofactors such as Magnesium, Calcium, Zinc or Vitamin A which are all needed to make Vitamin D.
Key Take Aways
- It is important to get key tests at the right time during your menstrual cycle – for some tests during the Follicular phase, for others the Luteal phase
- Don’t just focus on your hormone levels – assess and optimise your overall health too as this will also impact your fertility
- If living with a diagnosed condition or taking medication, speak to your GP as both of these can impact on fertility and pregnancy
The next and final blog in this series covers supplements for fertility and pregnancy and ways to maximise absorption.
If you have any questions about any information in this blog, get in touch.
I am happy to discuss the contents of this blog and run through the sources used and where you can find out further information.
My FREE guide 16 Ways to Boost your Fertility Naturally to get Pregnant covers lots of other ways to boost your fertility levels
Download Here